Chronic Venous Insufficiency (CVI) is a long-term condition in which the veins, most commonly in the legs, struggle to send blood back to the heart efficiently. Healthy veins contain one-way valves that prevent blood from flowing backward. When these valves weaken or fail, blood can pool in the lower extremities, leading to increased pressure in the veins, swelling, discomfort, and even skin changes like discoloration or thickening. Over time, untreated CVI can also result in venous ulcers, which are open sores that may become infected.
Many patients wonder whether CVI itself can be fatal. The simple answer is that CVI rarely causes death directly. However, it can lead to complications that are serious or even life-threatening if ignored. Chronic venous insufficiency should therefore be treated as a marker of long-term vascular health, not just a cosmetic or minor discomfort issue.

How CVI Can Lead to Serious Complications
While CVI primarily affects the veins in the legs, chronic blood pooling and high venous pressure can have far-reaching effects. Poor circulation over time weakens tissues, slows healing, and increases the risk of infection. Key complications include:
- Venous leg ulcers: These ulcers are often slow to heal because the surrounding tissue lacks adequate oxygen and nutrients. If bacteria enter these open wounds, it can lead to systemic infections that may spread beyond the leg.
- Severe skin infections (cellulitis): Persistent swelling and skin breakdown make patients vulnerable to cellulitis, a bacterial infection that can rapidly spread through the skin and bloodstream.
- Deep vein thrombosis (DVT): Blood clots may form in the deep veins of the legs due to stagnant blood flow. If a clot breaks off and travels to the lungs, it can cause a pulmonary embolism, which can be fatal without prompt treatment.
- Mobility issues: Chronic pain, swelling, and ulceration can limit movement, which may worsen cardiovascular health and increase the risk of clot formation.
These complications show that while CVI itself is rarely fatal, its consequences can be serious. Regular monitoring and early intervention are essential to prevent these outcomes.
Connection to Overall Circulatory Health
Chronic venous insufficiency (CVI) rarely exists in isolation. In most cases, it occurs alongside other vascular or heart conditions, such as coronary artery disease, high blood pressure, diabetes, or obesity. Poor venous circulation can act as an early warning sign of systemic vascular dysfunction, indicating that other parts of the circulatory system may also be compromised.
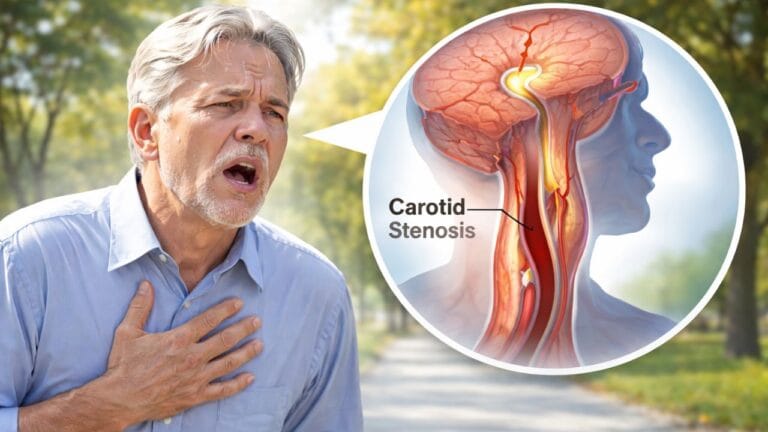
Patients with vascular disorders often notice overlapping symptoms and ask questions like Can carotid stenosis cause shortness of breath, because both arterial and venous problems can affect blood flow, oxygen delivery, and overall cardiovascular function. These shared circulatory challenges highlight how interconnected the venous and arterial systems are.
Understanding CVI in the context of overall vascular health is essential. Focusing only on the veins in the legs without addressing systemic factors may limit treatment effectiveness. Comprehensive care involves managing weight, maintaining cardiovascular fitness, controlling blood pressure and diabetes, and monitoring heart health.
Additionally, some patients experience blood pressure fluctuations or dizziness due to compromised vascular function, raising concerns such as can carotid stenosis cause orthostatic hypotension. Recognizing and addressing these coexisting conditions ensures that CVI management is safe, effective, and tailored to each patient’s overall circulatory health.
When Chronic Venous Insufficiency Becomes an Emergency
Although CVI is often manageable, it becomes more dangerous if warning signs are ignored. Patients should seek immediate medical attention in the following situations:
- Non-healing or rapidly worsening leg ulcers: Slow-healing wounds are prone to infection, which can spread into the bloodstream.
- Sudden leg pain, swelling, warmth, or redness: These are potential signs of deep vein thrombosis (DVT), a serious condition that can cause pulmonary embolism.
- Fever, chills, or spreading redness on the legs: These indicate a bacterial skin infection (cellulitis), which requires urgent antibiotics.
- Shortness of breath, chest pain, or dizziness: These could signal a pulmonary embolism or cardiovascular complications, especially if you also have coexisting heart issues.
CVI patients who experience these symptoms should not delay evaluation, as early treatment can prevent life-threatening outcomes.
Expert Medical Perspective
Vascular specialists, including Dr. Rema Malik, emphasize that CVI is more than a cosmetic issue or a minor discomfort. It reflects long-term stress on the circulatory system and is often an indicator of broader cardiovascular risk.
Medical management for CVI typically involves:
- Compression therapy: Compression stockings or bandages improve blood flow and reduce swelling.
- Lifestyle modifications: Regular exercise, leg elevation, weight management, and avoiding prolonged sitting or standing can improve circulation.
- Medications: Blood thinners or drugs that improve vein tone may be prescribed.
- Minimally invasive procedures: In some cases, endovenous laser therapy, radiofrequency ablation, or sclerotherapy can repair or close damaged veins.
By combining vein-specific treatments with overall cardiovascular care, most patients can prevent severe complications and maintain an active lifestyle.
Frequently Asked Questions (FAQ)
Can chronic venous insufficiency be fatal?
CVI itself is rarely fatal. However, untreated complications such as infections, DVT, or pulmonary embolism can become life-threatening.
How does CVI affect overall vascular health?
CVI often occurs alongside heart disease, diabetes, and arterial problems. Poor venous circulation can indicate systemic circulatory issues.
Can CVI cause shortness of breath?
Not directly. But associated heart or vascular conditions may lead to breathlessness, similar to concerns in carotid stenosis can cause shortness of breath.
Can CVI cause dizziness or blood pressure changes?
CVI itself usually does not, but coexisting circulatory problems may raise questions like Can carotid stenosis cause orthostatic hypotension?
What should I do if I notice worsening CVI symptoms?
Seek prompt medical care for leg ulcers, sudden swelling, pain, redness, fever, or any signs of shortness of breath to prevent serious complications.
Key Takeaway
Chronic venous insufficiency is rarely fatal. However, ignoring it or leaving complications untreated can be dangerous. Early diagnosis and proper treatment are essential. Managing leg symptoms, controlling heart and vascular health, and addressing related conditions can prevent serious problems. With consistent care, most patients can live safely and comfortably.
References
- American Heart Association – Chronic Venous Insufficiency Overview
- Mayo Clinic – Venous Insufficiency: Causes, Symptoms, and Treatment
- National Heart, Lung, and Blood Institute – Venous Thromboembolism and CVI
- Clinical insights referenced by Dr. Rema Malik, vascular specialist